15.5 million Californians are at risk of losing their Medi-Cal benefits if they don’t act now.
Between June 2023 and May 2024, more than 15 million Medi-Cal recipients will have their Medi-Cal eligibility redetermined as part of what’s been referred to as the “great unwinding.” In June 2023, 1,000,000 members were up for the redetermination process in California.
An alarming 225,000 individuals were disenrolled from Medi-Cal mainly because they did not return their redetermination packages or “yellow envelope” to the county for processing.
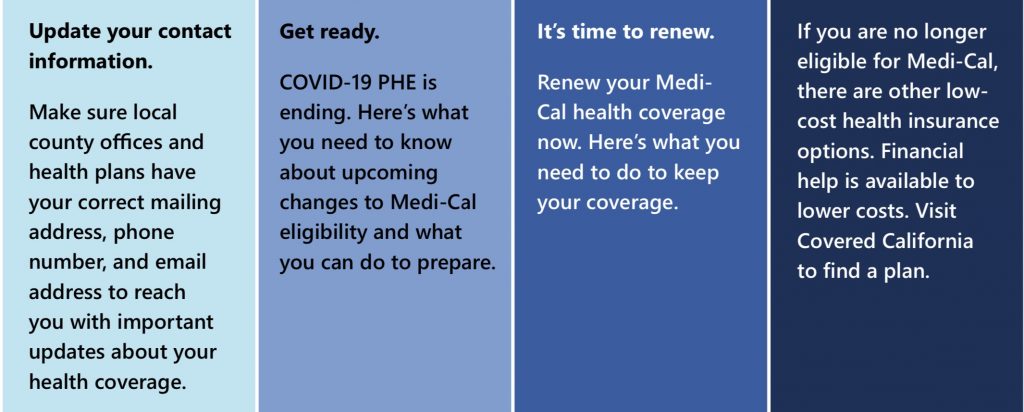
An average of 1 million residents will be up for redetermination each month during this 90 days process. Californians have until September 30, 2023, to take action to ensure that they keep their coverage, or transition to an option that they qualify for.
Related Links:
https://lasentinel.net/medi-cal-renewal-process-underway-across-california.html
https://lasentinel.net/heres-how-to-make-medi-cal-better-in-south-l-a.html
In January 2020, the U.S. Department of Health and Human Services (HHS) declared a Public Health Emergency (PHE) in response to the COVID-19 epidemic. Specific rules were established during the PHE to allow more people to either gain access to Medi-Cal or keep their existing coverage. The PHE has been renewed every 90 days since COVID-19 arrived in the United States.
Prior to COVID-19, the State of California would do an annual redetermination by reviewing and requesting updated information from Medi-Cal recipients. If the beneficiary is determined to be qualified, then their participation would be renewed for another year. But now that the PHE is officially over, the redetermination process is underway.
During a briefing sponsored by Ethnic Media Services, Yingjia Huang, deputy director of Health Care Benefits and Eligibility for California’s Department of Health Care Services (DHCS), explained, “DHCS is reviewing the eligibility of 15 million Medi-Cal enrollees. That’s more enrollees than any other state. We’re using this moment to really implement meaningful changes that will make it easier for our members to get and stay covered in the next year, and the next few years.”
She continued, “The Department of Health Care Services in California has disenrolled 21% of its Medi-Cal members who were redetermined in June. Many lost their benefits simply because they did not return their yellow packet. A portion of people who have been disenrolled have been moved to Covered California.”
The state has launched health enrollment navigators to make the process as seamless as possible. DHCS has an interactive dashboard that gives specific details on those who have been disenrolled. Enrollment navigators are people who have been trained to help anyone who finds the paperwork challenging to complete. The navigators will also receive continual training through March 2024.
Jessica Altman, CEO of Covered California, said, “California is well-positioned to help people keep health coverage during the ‘unwinding’ process. We do recognize that for many people, the process can be confusing, but we are here to help them. Californians who lose Medi-Cal coverage can get low or no-cost coverage through Covered California. Deductibles for them can also be eliminated.”
Altman noted that nearly 90 percent of Covered California’s over 1.6 million enrollees receive financial help and 2/3 of the enrollees pay $10 or less per month for their health insurance. Still, she acknowledged that some people still have trouble transitioning from Medi-Cal to Covered California.
Despite that reality, Altman insisted, “We are offering more financial assistance than ever before, empowered by the American Rescue Plan, and will offer even more assistance in 2024 as we implement a state program that will eliminate deductibles for any enrollee under 250% of the federal poverty level. Also, assistance is based on a household’s income.”
Louise McCarthy, CEO of the Community Clinic Association of Los Angeles County, added, “Community health centers are the key to keeping people enrolled. We can help people get through the bureaucracy.”
Other speakers included Dr. Seciah Aquino of the Latino Coalition for a Healthy California and
Mayra Alvarez of The Children’s Partnership. Both professionals encouraged enrollees to respond to the “yellow envelope from Medi-Cal” or any correspondence from L.A. County.
To learn more, visit https://www.dhcs.ca.gov/Pages/Keep-Your-Medi-Cal.aspx or watch “Top Things You Need to Know About Medi-Cal Renewal” at https://youtu.be/NVlhGArNMdA.
More information is available at https://www.dhcs.ca.gov/dataandstats/Pages/Continuous-Coverage-Eligibility-Unwinding-Dashboard.aspx and