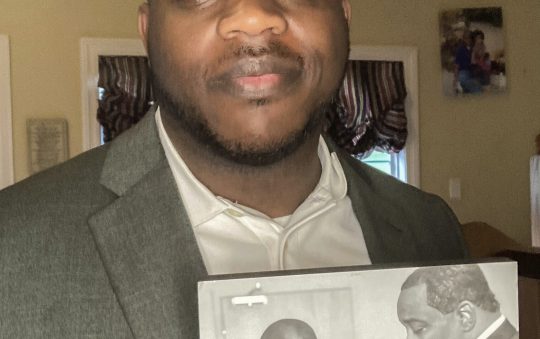
Q&A with Dr. Oscar Alleyne, Senior Advisor for Public Health Programs National Association of County and City Health Officials (NACCHO).
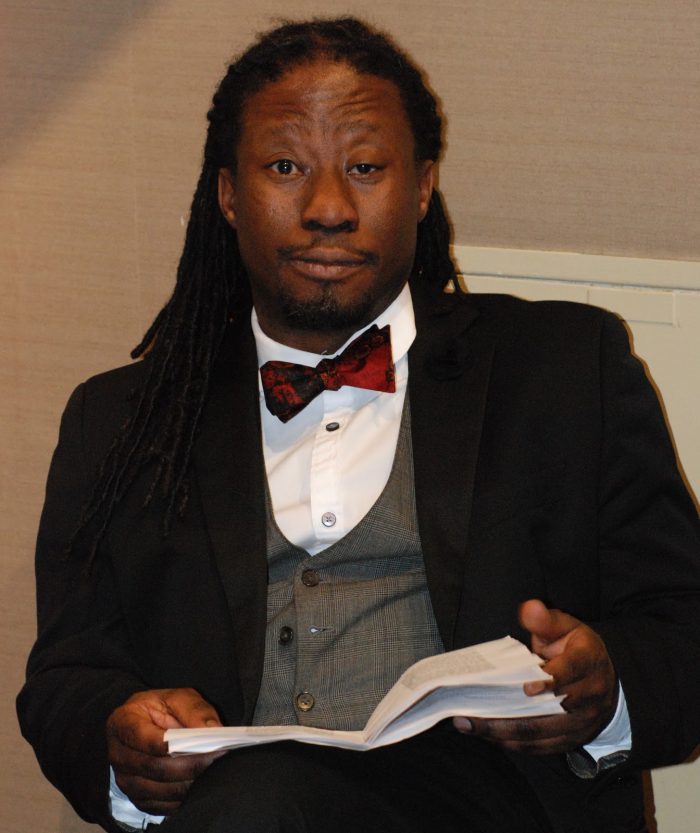
The Centers for Disease Control and Prevention (CDC) recently reported that 10 percent of the 250 women in the United States who had confirmed Zika infection in 2016 delivered a fetus or baby with Zika-related birth defects. In addition, 44 states reported pregnant women with evidence of Zika in 2016. The CDC also reported that only 1 in 4 babies with possible congenital Zika infection were reported to have received the recommended brain imaging after birth. Clearly, Zika is a serious public health issue. The following is a conversion with NACCHO epidemiologist Dr. Oscar Alleyne about what local health departments are doing to protect pregnant women and their babies.
Q. Dr. Alleyne, we know that Zika infection was an issue last year and Americans living in Gulf Coast states were particularly at risk from mosquito bites. Why is Zika infection still a threat in 2017?
Unfortunately, some have the misconception that Zika has disappeared because of the winter. While cold weather does reduce the risk of transmission by mosquitoes, we know that Aedes aegypti mosquito eggs are very resilient and can survive harsh conditions. In our southern-most states, the threat has not gone away, and we have seen positive cases of Zika transmission in Texas within the last month, because travel-related cases of Zika continue to occur.
Adding to the equation, this is a virus that continues to provide new revelations with its ability to be spread through sex and, even in one fatal case, by casual physical contact. There is great concern with the known birth defects like microcephaly, neurological damage and more recently, Zika-related seizures and epilepsy among infants born to mothers infected with the virus while pregnant.
Q. We have heard that local health departments’ use of vector control is very important. Please define a vector and tell us why control is so important.
A vector is a living organism that can transmit infectious diseases between humans, or from animals to humans. In the case of Zika, that vector is mainly the Aedes aegypti and Aedes albopictus mosquitos. Vector-control plans focus on using techniques proven to reduce mosquito populations.
Many of these actions try to manage the different stages of a mosquito’s life cycle. This includes tracking mosquitoes where they lay their eggs, killing mosquito larvae before they become biting adults, and using registered insecticides to kill adult mosquitoes. Fully competent control programs carry out tests for resistance to see how successful their insecticide applications worked in reducing the adult mosquito populations.
Q. If you live in an area where the local health department has all of the equipment and funding they need to protect residents, does that mean pregnant women shouldn’t be worried about possible infection?
Zika can be passed from a pregnant woman to her fetus and can cause serious birth defects. Women who are pregnant and women who are planning to become pregnant should know their risks and take the necessary precautions. Just because a community’s local health department is well-equipped and has sufficient funding to fight the disease does not mean pregnant women should not be worried about possible infection. NACCHO conducted a vector-control competency assessment and found that 68% of the vector- control programs that responded were in need of improvement.
Q. Can you tell us about strategies that some local health departments have used to reduce the chances of Zika infection for residents?
Local health departments across the United States have been exceptional in their response to Zika. This is seen in the community health worker engagement with residents that live in border communities like in the city of Laredo and Hildago County, Texas; to forming strong partnerships with municipalities and universities in creating contingency plans in Oklahoma City, Oklahoma; to testing exciting new mosquito trap technologies with Microsoft in Harris County, Texas; to the New York City Practice Safe Sex campaign that is translated into many languages, and urges New Yorkers to remain vigilant; to increased testing and family counseling available for children and families affected by Zika in Florida; to the deployment of CDC-hired local public health nurses to assist with the Zika Pregnancy and Birth Defect Registry in areas including Chicago, Salt Lake County, Alameda County, San Diego, Washington, D.C., and Palm Beach County.
Q.What can our local health departments do to increase awareness of Zika virus transmission to the public and healthcare providers?
Our local health department leaders continue to show their commitment to education and partnership in the spirit of public health protection. Many agreed to ramp up public education efforts to lower the chances of mosquito bites. Dallas County has developed emergency document bags with Zika information for residents and businesses. Laredo City health department clinicians, epidemiology, preparedness response, and nursing staff are wearing “Ask Me About Zika” tags and are working with local ob-gyn providers to encourage community awareness.
In Miami, a campaign to continue to educate the public on how to prepare to fight the bite include, for example, the importance of draining a plentiful and popular decorative plant: bromeliads. Bromeliads can hold water between their leaves, making them a great place for mosquitoes to breed. The interaction of medical, epidemiology, vector control, and maternal and child health is critical to all of these efforts, coupled with a strong spirit of collaboration.
Q. What type of federal funding is needed to continue to protect the public from Zika?
Zika funding is not where it should be, if we want to be serious about protecting the lives of our citizens. The current Administration’s proposed budget would eliminate one-eighth of the CDC’s budget. The budget for the Epidemiology and Laboratory Capacity (ELC) program is also proposed to be cut in half, and that directly threatens the Zika funding available to fight this disease. The reality is that vector control is done at the county and municipality level and there is a greater need for financial support to preserve and strengthen the public health infrastructure. We need to move the dial of our vector control programs from “in need of improvement” to being “competent and fully capable” to fight Zika.
In another example, congressional funding for the Zika Pregnancy and Birth Defect Registry was for one year. While it was able to execute some activities, the reality is that this one-time investment will go away. The end result of failing to fund this important surveillance system can be catastrophic. Babies infected by Zika will not be tracked, and connection to support and health services will disappear.
The delayed funding for Zika last year placed our public health system at a disadvantage to a rapidly changing outbreak. So understanding the overall burden placed on the other services is important, if we are to save lives and make an impact.
Q. Alleyne, you have many years of experience as an epidemiologist and former local health department director dealing with mosquito-borne illness and other epidemics. What surprises you about Zika and our response to it?
Even though we have learned that Zika — normally a mosquito-borne illness that now can be spread by sexual contact — causes birth defects and other neurological disorders, and with over 41,000 cases identified in the United States and territories, what surprises me is that we still have to prove that Zika is a public health threat. The projected costs of taking care of a child with birth defects from Zika is terribly high. They include the money needed to pay for special schooling, for home and lifestyle modifications, and high total medical lifetime costs. Yet still, the message is not resonating as widely as it should be. So it is not so much a surprise as it is a fear: a substantial fear that the battle may be lost if we do not fight the bite.